Dairy farms deliver: Antibiotic use on the decline while new alternatives remain on the uptick
Acting on the root cause of livestock diseases.

Keeping livestock free from infectious disease has been a concern since the first sheep and goats were domesticated in Mesopotamia almost 10,000 years ago. Sick animals produce less food, pose a risk to humans that consume their meat and milk, and threaten the health of the entire herd by spreading the contagion. After struggling to fight infection by quarantine and natural remedies, livestock producers began using antibiotics in the last century to combat disease with unprecedented efficiency.
However, with antibiotic resistance threatening to undermine the past 70 years of progress, another novel set of tactics is needed to ensure food security and safety. Michigan State University (MSU) AgBioResearch scientists from the College of Veterinary Medicine are working to develop new techniques aside from conventional antibiotics to fight and prevent diseases on the farm.
MSU associate professor of large animal clinical sciences Bo Norby has been studying antibiotic resistance on and off since graduate school. He began as a Ph.D. student at MSU measuring the impact of antibiotic elimination of resistance levels of bacteria in pigs raised on organic farms versus those raised on conventional farms.
“I think we were hoping it would be more of a slam dunk, with respect to lowering resistance, than it was,” he said. “It certainly has an impact, but on the other hand, it’s taken decades to reach the levels of resistance we currently see. It was probably naïve of me to think it would just go away so quickly.”
John Kaneene, director of the MSU Center for Comparative Epidemiology studies the epidemiology and mechanisms of antibiotic resistance in both livestock and humans. One focus is on identifying the factors that cause resistance to form.
“By understanding the mechanisms and dynamics of antibiotic resistance, we can get a sense of the magnitude of the problem,” said the MSU professor of epidemiology.
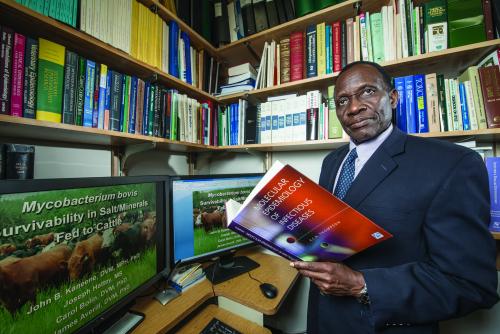 Kaneene has conducted research that found that regularly using antibiotic-medicated milk replacers on calves plays a role in resistance levels. Milk replacers are commercial substitutes for whole milk that are commonly used to feed calves on farms because they are typically less expensive and have less risk of contamination than whole milk. Taking a sample of Michigan dairy farms, all of whom initially fed calves with antibiotic-medicated milk replacers, Kaneene divided them into two groups. One group continued to use the medicated replacers, and the other switched to replacers without antibiotics. Kaneene and his team took samples from the animals and environments of each farm over the course of one year and found that, in the group without antibiotics, resistance had decreased.
Kaneene has conducted research that found that regularly using antibiotic-medicated milk replacers on calves plays a role in resistance levels. Milk replacers are commercial substitutes for whole milk that are commonly used to feed calves on farms because they are typically less expensive and have less risk of contamination than whole milk. Taking a sample of Michigan dairy farms, all of whom initially fed calves with antibiotic-medicated milk replacers, Kaneene divided them into two groups. One group continued to use the medicated replacers, and the other switched to replacers without antibiotics. Kaneene and his team took samples from the animals and environments of each farm over the course of one year and found that, in the group without antibiotics, resistance had decreased.
Though the initial results looked promising, Kaneene said that soon changed. Those farms eventually began to experience a resurgence of resistance. Like Norby, Kaneene found that simply eliminating the use of antibiotics was not enough— new techniques would be needed. Currently, he is in the beginning stages of research to investigate new treatments for gastrointestinal disease in cattle that do not involve antibiotics.
“In some cases, you can minimize antibiotic use, which helps us to reduce the formation of resistance on the farm,” Kaneene said.“That’s just a starting point, however.”
Norby, who returned to MSU in 2011 this time to work, renewed the efforts he began while a doctoral student to examine antibiotic-resistant Escherichia coli in dairy cattle. By subjecting samples of E. coli to a battery of 14 to 16 antibiotics, Norby was able to quantify the level of resistance it had to various antibiotics.
“We had to understand the quantity of resistance in the bacteria before we could assess the impact of different interventions in the animals,” Norby explained. “I was bothered. When we began researching resistance, we found that cutting out antibiotics was not the quick-fix solution. When I came back to MSU, we started looking for alternatives to stopping cold turkey.”
Norby began testing a variety of substances to create products that can be injected into the udder of a cow like an antibiotic. He is particularly optimistic about the potential of honey derived from the nectar of the manuka tree, which has natural antibacterial and tissue-repairing properties, as well as oregano.
“The hope is to find something that will give dairy producers a non-antibiotic option for treating their animals,” Norby said.
The first step in determining a substance’s viability is to test it against isolated strains of bacteria in the lab. Norby exposes a sample of bacteria to increasing amounts of a candidate until he finds the point at which it prevents bacteria from growing, known as the minimum inhibitory concentration.
The candidate must also be tested for safety. Norby’s team will first shave the fur from the portion of the cow’s udder and apply the candidate to the bare skin to test for inflammation. Next, it will be injected into the udder to ensure it does not make the animal sick or cause more inflammation, thereby exacerbating the illness it was designed to treat. Only after these rounds of testing can it move to the clinical trial stage, where multiple candidates are tested both against one another and against an already medically approved antibiotic to determine which of the alternatives is most effective.
Finding alternatives to traditional antibiotics represents an important middle ground in reducing antibiotic resistance, Norby said.
“When we use antibiotics, even only when we’re clinically supposed to, we affect the levels of resistance in the animals and environments in which we use them,” he said. “By having alternatives, we take some of that selective pressure away and slow the propagation of resistance.”
New practices for a healthier farm
 While Norby and Kaneene study alternative medical treatments to antibiotics, other MSU researchers are approaching the issue from a different angle. They are examining livestock practices that promote better animal health and maximize the efficacy of the immune system to reduce the incidence of disease and, therefore, the reliance on antibiotic therapy.
While Norby and Kaneene study alternative medical treatments to antibiotics, other MSU researchers are approaching the issue from a different angle. They are examining livestock practices that promote better animal health and maximize the efficacy of the immune system to reduce the incidence of disease and, therefore, the reliance on antibiotic therapy.
MSU AgBioResearch veterinarian Ronald Erskine’s research focuses on mastitis, a bacteria-caused inflammation of the cow’s udder and the most common disease to afflict dairy cattle in the United States. According to the U.S. Department of Agriculture, mastitis affects 15 to 20 percent of Michigan dairy cows annually. For an average-size dairy farm of 187 cows, the disease can result in the annual loss of about 25,000 pounds of milk and an annual cost of up to $10,000 in medical treatment. Severe cases can result in even greater losses along with long-term impacts on the health, welfare and fertility of the affected animals.
“Mastitis is caused by white blood cells moving into the udder to fight an infection,” Erskine explained. “It’s not much different from when you have a head cold — that’s when your immune system responds to an invading bacterium or virus. So when we’re talking about mastitis, we’re talking about the classic signs of immune response: inflammation, redness, soreness.”
As the most common disease in dairy cows, mastitis is likewise the most common reason for antibiotic use on dairy farms. Erskine has dedicated much of his career to finding new ways to combat the illness.
“Mastitis is a problem dairy producers have to tackle every day,” Erskine said. “They have to make a choice to treat a cow with antibiotics or not. From the standpoint of both productivity and cow well-being, the goal is to reduce mastitis, and we’re trying to find the most effective ways of doing that.”
Part of Erskine’s research is determining when antibiotic therapy is an appropriate tactic. Mastitis is caused by a wide range of bacterial pathogens, not all of which are susceptible to antibiotics. The most common agents of mastitis, streptococci and staphylococci, respond very well to antibiotics if caught in time. Other causes, however, do not.
“Much like the debate that goes on with pediatricians or doctors when you have a cold, the question is do you want to jump in and start with antibiotics?” Erskine said. “We try to help dairy producers and their veterinarians make informed decisions on when it’s appropriate to use antibiotics and when to wait and see if the cow’s own immune system can fight it off. It’s all about prudent, judicious use of antibiotics, using them only when they’re necessary.”
To determine whether the case is treatable with antibiotics, Erskine conducts bacterial cultures of milk from the infected cows to determine the type of bacteria causing the disease.
“It’s no different than what happens at a hospital,” Erskine said. “If you have strep throat, somebody collects a swab and identifies the organism before they give you antibiotics.”
The other key aspect in determining whether to use antibiotics is to understand the medical history of both the entire herd and the individual cows within the herd. Some bacterial infections can cause a chronic change in the cow udder, producing scar tissue and becoming more difficult to treat.
“You try to treat these infections as soon as you can, but sometimes they become chronic,” Erskine said. “We try to help farmers make the right choices based on records of the cow’s health. For instance, maybe we’ve treated a cow before and it didn’t work. The question then becomes: do we really want to keep using antibiotics on this cow, or do we recognize her as a poor candidate for this kind of therapy?”
 Erskine believes that training practices on the farm are an effective means of improving animal health while reducing reliance on antibiotics. As farms have dramatically increased productivity levels in the past two decades, he said producers have become increasingly reliant on employees to manage the expanded herds.
Erskine believes that training practices on the farm are an effective means of improving animal health while reducing reliance on antibiotics. As farms have dramatically increased productivity levels in the past two decades, he said producers have become increasingly reliant on employees to manage the expanded herds.
“The classic story you’ll hear is that when Dad took over the farm from his father in the ’80s, they had 100 cows,” Erskine said. “Now, in 2014, he has 300 or 400 cows, six full-time and three part-time employees.”
In addition to increased production, this expansion of farm personnel has introduced new challenges to the industry.
“We have a very progressive dairy industry in Michigan, when you look at our ranking in terms of milk production and quality,” Erskine said. “We have a group of producers that are very good at what they do — this goes beyond mastitis to how cows are housed, fed, bred, everything — but I think there are challenges in managing labor. All of a sudden they’ve gone from dealing with farm issues among immediate family to having to manage 10 or 15 people. The more people you have, the more variance there is from protocol, and that increases the risk of diseases appearing.”
Establishing and following protocols for the daily operations of a dairy farm, from milking procedures to administering antibiotics to preparing feedstocks, is paramount to a healthy herd. To help producers and their employees implement and follow farm protocols, Erskine leads a multi-institutional research team developing training programs that engage employees with farm owners, managers and veterinarians.
A survey of dairy farm employees revealed a strong desire to be trained on how, as well as why, to perform farm operations. “We have a belief that, if employees are engaged like this, protocol drift will be reduced and incidences of things like mastitis are going to come down,” Erskine said.
On the basis of a survey of the concerns and practices of more than 600 producers in Michigan, Florida and Pennsylvania, Erskine’s team crafted an evaluation system to develop protocols and educational materials to help veterinarians educate farm employees.
“We’re going to help people set goals, communicate and find ways to educate employees to generate long-term change,” Erskine said. “We’re all learning here. This is a new environment for dairy farmers and we’re all just trying to find the right dance partners, so to speak.”
Fighting disease by promoting health
 Animals, including livestock, were fighting bacterial infections long before the dawn of antibiotics. Under the right conditions, the immune system serves as a formidable defense against disease. MSU professor of large animal clinical sciences and bovine immunology specialist Lorraine Sordillo is developing ways to bolster the immune system through a cow’s environment and diet to reduce mastitis and other infections on dairy farms.
Animals, including livestock, were fighting bacterial infections long before the dawn of antibiotics. Under the right conditions, the immune system serves as a formidable defense against disease. MSU professor of large animal clinical sciences and bovine immunology specialist Lorraine Sordillo is developing ways to bolster the immune system through a cow’s environment and diet to reduce mastitis and other infections on dairy farms.
“It’s not that antibiotics are a bad thing, but we don’t want to use them arbitrarily,” Sordillo said. “The best way of reducing the need for them is to prevent the disease from occurring in the first place.”
When cows are stressed, the capabilities of their immune systems become diminished and the incidence of illnesses rises. Sordillo’s research aims at reducing that stress.
“The focus of our research is to understand the mechanisms that compromise the animal’s immune system and try to come up with intervention strategies that bolster the immune system during times of increased exposure to mastitis-causing pathogens,” Sordillo said.
The many ways to strengthen the immune system range from vaccines to dietary adjustments. Because of the sheer variety of bacteria that cause infections such as mastitis in dairy cows, the effectiveness of vaccination is limited because it targets individual strains of bacteria.
Instead of vaccination, Sordillo looks at changing nutritional and metabolic conditions to reinforce the bovine immune system.
Among the most stressful periods is the birthing of a calf and the initiation of milk production. Some changes in the ways cows use available nutrients during this time can suppress immune function, leaving them susceptible to disease. Through improved nutrition, Sordillo has found ways to mitigate the negative effects of this altered nutrient metabolism.
“We want to make sure the cow’s dietary intake is optimized because that reduces stress on the body and the need to metabolize fat stores,” Sordillo said. “A lot of energy is expended in the calving process and at the onset of lactation. For a cow to be able to meet those energy demands, she has to consume enough feed. If not, then she’s going to start mobilizing her tissue stores to release fats for energy.”
The mobilization of fats introduces free fatty acids into the bloodstream, which represses the immune system. Ensuring that cows have enough energy from their feed reduces this mobilization, and the immune system remains intact.
The energy consumed during lactation also results in the production of metabolic waste called reactive oxygen species. These molecules, natural byproducts of energy consumption in the body, are highly toxic in the high quantities present during milk production, and coping with this accumulation of toxins strains the cow’s antioxidant defenses. This can be exacerbated during periods of infection, when the immune system produces further quantities of reactive oxygen species in order to kill bacteria.
Sordillo’s research indicates that increasing the dietary concentration of antioxidant nutrients such as selenium and vitamin E during early lactation may mitigate the harm caused by these molecules.
“The production of reactive oxygen species is a natural part of metabolism and a normal response of the immune system, but, like anything, the problem comes when there’s too much,” Sordillo said. “In order to get back to normal levels, you have to increase the antioxidants the cow is receiving. When you don’t, the toxins can not only damage tissues but have a profound effect on the immune system, and that’s a major factor in disease susceptibility.”
Better health through better treatment
Eight millennia after the first livestock were domesticated, Plato wrote that necessity is the mother of invention. Though the venerable philosopher was referring to the politics of ancient Greece, his words ring true for the work of MSU AgBioResearch scientists examining livestock health. With the development of resistance, unilateral antibiotic therapy is no longer a viable option for disease treatment.
“The development of new antibiotics in no way keeps up with the potential development of antibiotic-resistant bacteria,” Sordillo said. “The bacteria are far faster at adapting than we are at developing new antibiotics.”
The development of alternative treatment strategies has already led to techniques not only to treat diseases but to help prevent them. There will always be cases that require antibiotic therapy, but these new practices reduce the need.
“When you look at the overall trend here in Michigan, and even nationally, antibiotic use has been steadily declining in dairy,” Erskine said. “Our producers have been working hard at that, and with the new techniques and technologies we’re developing, they’re going to be able to do even better.”



 Print
Print Email
Email