Striving to stave off antibiotic resistance
MSU researchers work to identify new antibiotics and more effective therapies.
Numerous Michigan State University (MSU) researchers are working to identify new antibiotics and treatment methods to combat life-threatening bacterial infections. Their work comes at a critical time when bacteria have demonstrated an ability to develop resistance to every known antibiotic, and new antibiotic development has been nearly non-existent for more than 30 years.
“[Universities] tend to be able to take more risks with our research and pursue projects that companies deem too risky,” said Richard Neubig, chair of the MSU Department of Pharmacology and Toxicology.
“With the students and resources the university has available, researchers are able to ask questions that just wouldn’t be asked in industry,” Neubig said. “We may end up exploring 20 to 30 different areas, and a large fraction of those may fail. But the one that hits, can really let us move in new and exciting directions.”
While high costs have deterred many pharmaceutical companies from investing in new antibiotic development, MSU is uniquely positioned to lead the way due to its vast expertise in the colleges of Agriculture and Natural Resources, Human Medicine, Natural Science, Osteopathic Medicine and Veterinary Medicine, to name a few.
“Drug discovery is a team sport,” Neubig said. “Support from the MSU Foundation’s Strategic Partnership Grants has brought together an exciting team from plant biology, drug discovery and microbiology to find unique compounds to tackle important antimicrobial resistance problems like methicillin resistant Staphylococcus aureus, or MSRA, and other resistant microbes.
“When we can bring all of these different aspects together, it allows us to attack problems in ways that hasn't been done before.”
Eliminating antibiotic “shields”
Christopher Waters, professor in the MSU Department of Microbiology and Molecular Genetics, is striving to develop antibacterial therapies through his research on bacterial biofilms. Biofilms are generated by bacterial colonies that attach to surfaces and secrete material that shields the bacteria from environmental stresses, including immune system response and antibiotics.
Biofilms form in a variety of diseases, including diabetes, cystitis, infections from medical implants and cystic fibrosis.
“The bacteria form these chronic infections when they’re in the biofilms,” Waters explained. “As your body is trying to clear the biofilm, which it can’t successfully do, that site becomes very inflamed and is often one of the big causes of tissue damage.
“There are a couple of different approaches to treating bacterial infection,” he continued. “You can develop new antibiotics that have new targets. Or, you can take known antibiotics and add another compound to make the antibiotics work better against antibiotic resistant bacteria. Those compounds are called antibiotic adjuvants. We decided to go this route to see if we could develop antibiotic adjuvants specifically looking for antibiotic compounds that enhance the destruction of biofilms.”
Waters has screened approximately 6,000 molecules, testing their ability to attack and destroy biofilms. Several compounds have emerged as potential solutions. The most promising is triclosan when combined with the antibiotic tobramycin. Triclosan enhances the ability of tobramycin to kill the bacterial pathogen Pseudomonas aeruginosa, a major biofilm forming pathogen.
“We found that triclosan enhances antibiotics known as aminoglycosides,” he said. “Neither [triclosan or aminoglycosides] working alone against biofilms are very effective, but if you combine them they’re 100 times more effective.”
The compound has shown effectiveness in pneumonia and wound infections in animal trials.
“One of the best properties of [the triclosan/tobramycin compounds] is its broad-spectrum ability to kill a lot of different bacteria,” Waters said. “We think clinically for a lot of infections, like cystic fibrosis infections that are poly-microbial in nature, having something that can kill a lot of different things when they’re producing biofilms is pretty powerful.”
Waters said he hopes to ultimately treat a large number of biofilm-related illness.
“Diabetics often get infections in their lower legs and feet that can’t be cleared and often have to have their feet amputated,” he said. “We are hoping that our treatment will allow us to treat those infections and prevent people from having to lose limbs. If we can clear out the infection in the lungs in cystic fibrosis patients, we could also extend the life of those patients.”
Treating antibiotic resistance in TB
Tuberculosis (TB) is the leading cause of death from infectious disease. Caused by the bacteria Mycobacterium tuberculosis (MTB), TB results in one death every 20 seconds. Additionally, an estimated 2 billion people worldwide are infected with latent TB, which has no symptoms.
Robert Abramovich, associate professor in the Department of Microbiology and Molecular Genetics, is focused on identifying the dormant MTB that causes latent TB and developing new antibiotics to destroy the bacteria before it develops. He said identifying and eliminating latent TB is key to both preventing the illness and reducing resistance.
“TB treatment takes six months,” he said. “We can kill the bacteria that are replicating – that are active – pretty easily with antibiotics. The extended course is to make sure we clear out the bacteria that are dormant and harder to kill with antibiotics. This extended treatment, due to dormancy, leads to drug tolerance. If we can stop bacteria from establishing dormancy, we can stop creating drug tolerance.”
When an immune system senses MTB, it surrounds the infection and essentially starves the bacteria of oxygen, making it dormant.
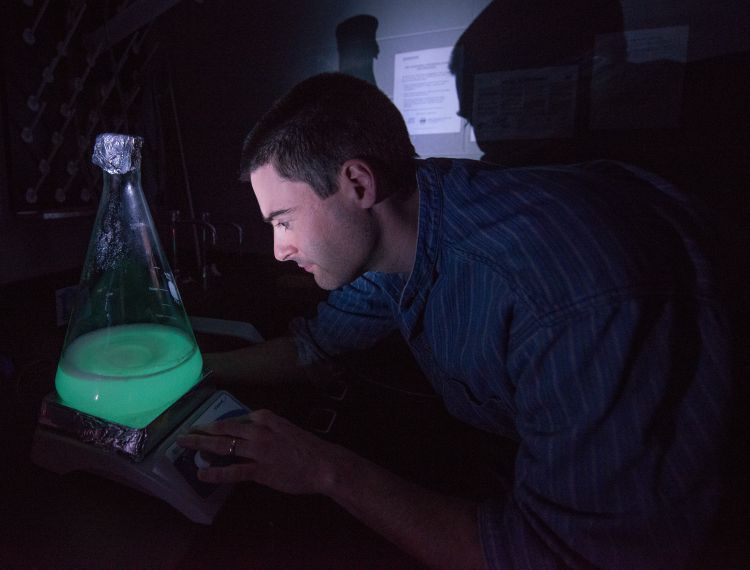
Abramovich received the 2014 MSU Innovation of the Year Award for developing a strain of MTB that produces a glow when it goes dormant. Since then, he and his research team have screened more than 250,000 compounds. In 2017, Abramovich published a paper identifying six compounds that successfully target dormancy and have the ability to destroy dormant TB in the lab.
“Artemisinin is one compound we are really excited about,” Abramovtich said. “We know how it works to inhibit dormancy pathways and now, we will use those dormancy findings to hopefully develop new antibiotics.”
Understanding dormancy was a major breakthrough for Abramovich. It allows researchers to test new compounds with an understanding of bacterial biology.
“Our six leading compounds for preventing dormancy might not be the right ones, but our research has given us the mechanism for how these bacteria operate,” he said.
Ultimately, Abramovich is hopeful that one of the compounds will go to clinical trials and eventually into production. Even so, it’s still an upward battle.
“Bacteria will always evolve resistance,” he said. “We need new antibiotics that can develop into more efficient therapies to shorten the course of therapy to slow down the evolution of resistance.”
High-throughput lab accelerating research
Abramovich credits the role Neubig, his colleague in the College of Natural Science, and the MSU Drug Discovery Program for testing thousands of compounds in its high-throughput screening lab. The Assay Development and Drug Repurposing Core (ADDRC) in the Department of Pharmacology and Toxicology assists MSU researchers with drug discovery. It is a campuswide resource that provides expertise in screening compounds, especially those relevant to the fields of biology and biochemistry, at a very rapid rate.
“When I came to MSU six years ago, I received tremendous help from the university to build the high-throughput screening lab – the ADDRC – and, more recently, the Medicinal Chemistry Core (MCC) that are needed to take compounds we find, optimize them and make them viable as potential drugs,” Neubig said.
Thomas Dexheimer, ADDRC director, who brings critical expertise in preclinical drug discovery, and Edmund Ellsworth, MCC director, who spent decades working on drug development in the pharmaceutical industry, are leading the way on assisting researchers across campus, according to Neubig.
“It’s been a lot of fun to talk to scientists, who have very different areas of expertise,” he said. “You learn so much from these collaborations, and by bringing together people who wouldn’t normally work together. You can explore completely new areas that really provide novelty and innovation that you wouldn’t get without the collaboration.”
Two leading scientists in the MSU Department of Microbiology and Molecular Genetics, Victor DiRita, Rudolph Hugh Endowed Chair in microbial pathogenesis, and Neal Hammer, assistant professor, are also using the ADDRC and the MCC, to fuel their research.
“We are moving toward precision-based targeting where we discover how the bacteria function in order to disarm them, not necessarily to kill them,” said DiRita, whose lab studies the Gram-negative bacteria devastating hospitals known as Carbapenem-Resistant Enterobacteriaceae (CRE). “This approach is smart and targeted — this is a laser beam, not a sledgehammer.”
DiRita’s lab will sift through the ADRCC library of plant-inspired compounds to identify those that limit in vitro growth of CRE, then target the pathways that lead to colonization of the bacteria in order to assess expression of genes essential in sepsis development.
“With some microbes, we have identified small, potentially therapeutic molecules that stop the production of an important toxin by understanding the important microbial pathways that turn on toxins and cause the host problems,” DiRita explained. “This next generation of antibiotics won’t kill bacteria — they will protect it from being lethal.”
The Hammer lab aims to limit the infectious capacity of the Gram-positive pathogen methicillin-resistant Staphylococcus aureus, or MRSA, by screening MSU’s growing library of new plant-based compounds for ones that will inhibit its metabolic pathways.
“Through our research, we know that S. aureus has an interesting pathway of becoming resistant to several classes of antibiotics – it switches its metabolism to a small colony variant, or SCV,” Hammer said. “This is somewhat good news because our work, and work done by many other labs, demonstrated that S. aureus only uses two metabolic pathways to proliferate during infection, aerobic respiration and fermentation. SCVs rely on fermentation.”
Metabolically speaking, S. aureus is somewhat similar to humans. When we exercise, oxygen become limiting and lactic acid is produced via fermentation — hence sore muscles. S. aureus, in SCV form, also makes lactic acid as a fermentative end-product.
“We can force S. aureus into a fermentative, SCV state with a class of drug treatment called aminoglycocides,” Hammer said. “My research program is interested in finding compounds in our chemical library that selectively kill these SCVs to design a combinatorial therapy that potentiates the activity of the aminoglycocides.”
“Fundamentally, we are biologists who are curious about bacteria and how they work and, if they are harming people, how we can stop them from working,” DiRita added. “If this is a space race, we are John Glenn circling the earth. These are the early days for this type of research, and MSU, thanks to the MSU Foundation, is leading the way.”
Vaccines providing alternative
MSU Biomedical Engineering and Chemistry Professor Xuefei Huang strives to provide a complementary approach to antibiotic discovery through his work on vaccines.
Huang is examining the role carbohydrates play in inflammation, tumor metastasis and both bacterial and viral infections. He strives to create vaccines for a variety of diseases, including bacterial infections.
“Our interest is finding a way to target carbohydrates to generate immune responses that will protect against bacterial infection,” Huang said. “The vaccine approach is complementary to antibiotics in the sense that the reason we are using a vaccine is to prevent the infection and antibiotics are used to kill the infection.”
The use of better vaccine therapy could also play a role in antibiotic resistance. If vaccines can boost the immune system enough to fight a bacterial infection, then antibiotic use would decrease.
“Creating new vaccines does not mean we shouldn’t develop new antibiotics,” Huang said. “I don’t think any one single lab can take on the task of eliminating infections successfully. At MSU, we are in a good position with the expertise we have on campus and the collaborative environment.”
Looking forward
The ultimate goal is to develop therapies far enough along to establish clinical trials and ultimately generate new antibacterial therapies. Abramovich believes that’s when the pharmaceutical companies can really step in and make a difference.
“I like to use a football analogy,” he said. “In academia, we can sort of get the ball down the field and into the red zone. At that point, to get a touchdown, you probably need some industry help to get it to the end zone. If we can get it to that point, industry has a good shot at succeeding.”
Waters has partnered with TSRL, Inc., based in Ann Arbor, to develop his triclosan/tobramycin compound.
“TSRL works with people in university settings with new technologies to bring those through pre-clinical development to get to a point to present to the FDA for clinical trial,” Waters said. “We’ve been working really hard with them over the last couple of years, looking at efficacy in animal models and developing formulation so we can have a safe treatment for patients.”
Waters, Abramovich and Huang have also each developed start-up companies designed to further their research into clinical trials and eventually, drug therapy production.
Abramovich is encouraged by the vast amount of talent MSU has working on the issue of antibiotic resistance.
“Over the past few years, one major change is we now have a corps of researchers, many of whom are new to the university, and all of them are leaders in their respective fields,” he said.
Waters said having diverse expertise is the best way to generate successful new treatments.
“It’s such a big task to do any sort of drug development and no one lab can do it alone,” he said. “I can be an expert in signaling and biofilms, but I really don’t know much about drug development. So, having people who know about drug discovery, such as Rick Neubig, Tom Dexheimer and Edmund Ellsworth, brings in a whole new perspective that I don’t have.
“It’s kind of like the triclosan and the tobramycin,” he said. “Either one alone is not that effective, but when you bring the two together – it works.”
Ultimately, the researchers agree that a combination of treatments will be required to continue to treat bacterial infection and prevent resistance.
“It doesn’t matter what the treatment is, you’re always going to have bacteria that evolve resistance at some point,” Waters said. “Having multiple strategies and multiple effective therapies is the best way to manage resistance.
“I think these combination strategies are really important,” he added. “You can treat bacteria with multiple therapeutics targeting different pathways and it becomes much harder for bacteria to evolve resistance at the same time.”
MSU College of Natural Science freelance writer, Sarah Zwickle, contributed to this article.



 Print
Print Email
Email